Test for the significance of relationships between two CONTINUOUS variables
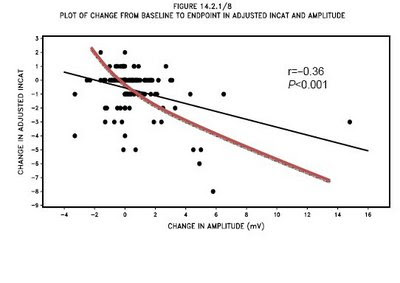
- We introduced Pearson correlation as a measure of the STRENGTH of a relationship between two variables
- But any relationship should be assessed for its SIGNIFICANCE as well as its strength.
A general discussion of significance tests for relationships between two continuous variables.
- Factors in relationships between two variables
The strength of the relationship: is indicated by the correlation coefficient: r
but is actually measured by the coefficient of determination: r^2
- The significance of the relationship
is expressed in probability levels: p (e.g., significant at p =.05)
This tells how unlikely a given correlation coefficient, r, will occur given no relationship in the population
NOTE! NOTE! NOTE! The smaller the p-level, the more significant the relationship
BUT! BUT! BUT! The larger the correlation, the stronger the relationship - Consider the classical model for testing significance
It assumes that you have a sample of cases from a population.
The question is whether your observed statistic for the sample is likely to be observed given some assumption of the corresponding population parameter.
If your observed statistic does not exactly match the population parameter, perhaps the difference is due to sampling error.
The fundamental question: is the difference between what you observe and what you expect given the assumption of the population large enough to be significant -- to reject the assumption?
The greater the difference -- the more the sample statistic deviates from the population parameter -- the more significant it is.
That is, the lessl ikely (small probability values) that the population assumption is true. - The classical model makes some assumptions about the population parameter:
Population parameters are expressed as Greek letters, while corresponding sample statistics are expressed in lower-case Roman letters:
r = correlation between two variables in the sample
(rho) = correlation between the same two variables in the population
A common assumption is that there is NO relationship between X and Y in the population: r = 0.0
Under this common null hypothesis in correlational analysis: r = 0.0
Testing for the significance of the correlation coefficient, r
When the test is against the null hypothesis: r_xy = 0.0
What is the likelihood of drawing a sample with r_xy 0.0?
The sampling distribution of r is
approximately normal (but bounded at -1.0 and +1.0) when N is large
and distributes t when N is small.
The simplest formula for computing the appropriate t value to test significance of a correlation coefficient employs the t distribution:
t=r*sqrt((n-2)/(1-r^2))
The degrees of freedom for entering the t-distribution is N - 2
- Example: Suppose you obsserve that r= .50 between literacy rate and political stability in 10 nations
Is this relationship "strong"?
Coefficient of determination = r-squared = .25
Means that 25% of variance in political stability is "explained" by literacy rate
Is the relationship "significant"?
That remains to be determined using the formula above
r = .50 and N=10
set level of significance (assume .05)
determine one-or two-tailed test (aim for one-tailed)
t=r*sqrt((n-2)/(1-r^2))=0.5*sqrt((10-2)/(1-.25)) = 1.63
For 8 df and one-tailed test, critical value of t = 1.86
We observe only t = 1.63
It lies below the critical t of 1.86
So the null hypothesis of no relationship in the population (r = 0) cannot be rejected
- Comments
Note that a relationship can be strong and yet not significant
Conversely, a relationship can be weak but significant
The key factor is the size of the sample.
For small samples, it is easy to produce a strong correlation by chance and one must pay attention to signficance to keep from jumping to conclusions: i.e.,
rejecting a true null hypothesis,
which meansmaking a Type I error.
For large samples, it is easy to achieve significance, and one must pay attention to the strength of the correlation to determine if the relationship explains very much. - Alternative ways of testing significance of r against the null hypothesis
Look up the values in a table
Read them off the SPSS output:
check to see whether SPSS is making a one-tailed test
or a two-tailed test - Testing the significance of r when r is NOT assumed to be 0
This is a more complex procedure, which is discussed briefly in the Kirk reading
The test requires first transforming the sample r to a new value, Z'.
This test is seldom used.
You will not be responsible for it.