In clinical trials, reporting of adverse events is critical to ensure the safety of participants. When an adverse event is reported, it is also assessed for the severity, seriousness, causality, and outcome. All of these are the standard fields that are supposed to be collected on the case report forms and on serious adverse event (SAE) forms.
Expectedness of an adverse event is also critical; however, the assessment of expectedness is usually not collected on the case report form or SAE form because the responsibility of the expectedness evaluation is not on investigator’s side, but on the sponsor’s side. SUSAR (suspected unexpected serious adverse reaction) must be reported to regulatory agencies and IRBs in expedited way.
Definition of Expectedness: According to ICH E2A “
CLINICAL SAFETY DATA MANAGEMENT: DEFINITIONS AND STANDARDS FOR EXPEDITED REPORTING”, the unexpected adverse drug reaction is defined as the following:
3. Unexpected Adverse Drug Reaction An adverse reaction, the nature or severity of which is not consistent with the applicable product information (e.g., Investigator's Brochure for an unapproved investigational medicinal product). (See section III.C.)
In each individual study protocol, the definition may be a little bit different, but essentially the same.
Unexpected: – Not listed in Investigator Brochure or is not listed at the specificity or severity that has been observed, or, if an investigator brochure is not required or available, is not consistent with the risk information described in the general investigational plan or elsewhere in the current application.
An unexpected adverse reaction has a nature or severity of which is not consistent with the study intervention description (e.g. Investigator's Brochure for an unapproved investigational product or package insert/summary of product characteristics for an approved product). The unexpected AE must be reported, whether related to the study intervention or not, with as much detail as is available
Expected: - listed in Investigator Brochure.
The Purpose of Expedited Reporting of the Suspected Unexpected Serious Adverse Events (SUSAR)
According to ICH E2A “
CLINICAL SAFETY DATA MANAGEMENT: DEFINITIONS AND STANDARDS FOR EXPEDITED REPORTING E2A”, the purpose of the SUSAR reporting is defined as:
C. Expectedness of an Adverse Drug Reaction The purpose of expedited reporting is to make regulators, investigators, and other appropriate people aware of new, important information on serious reactions. Therefore, such reporting will generally involve events previously unobserved or undocumented, and a guideline is needed on how to define an event as "unexpected" or "expected" (expected/unexpected from the perspective of previously observed, not on the basis of what might be anticipated from the pharmacological properties of a medicinal product). As stated in the definition (II.A.3.), an "unexpected" adverse reaction is one, the nature or severity of which is not consistent with information in the relevant source document(s). Until source documents are amended, expedited reporting is required for additional occurrences of the reaction.
The following documents or circumstances will be used to determine whether an adverse event/reaction is expected: 1. For a medicinal product not yet approved for marketing in a country, a company's Investigator's Brochure will serve as the source document in that country. (See section III.F. and ICH Guideline for the Investigator's Brochure.) 2. Reports which add significant information on specificity or severity of a known, already documented serious ADR constitute unexpected events. For example, an event more specific or more severe than described in the Investigator's Brochure would be considered "unexpected". Specific examples would be (a) acute renal failure as a labeled ADR with a subsequent new report of interstitial nephritis and (b) hepatitis with a first report of fulminant hepatitis.
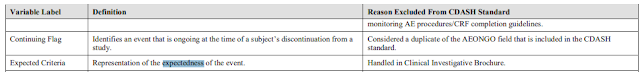
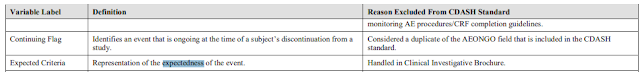
Expectedness/Unexpectedness Not Collected in Case Report Forms or SAE Forms CDISC/CDASH “
Clinical Data Acquisition Standards Harmonization (CDASH) User Guide” excluded the collection of ‘expected criteria’, citing that it is “handled in Clinical Investigative Brochure”
In FDA’s Guidance for Industry and Investigators “
Safety Reporting Requirements for INDs and BA/BE Studies”, the reporting responsibility for unexpected adverse events is specified for sponsors (not the investigators).
Two Types of Unexpectedness and Handling the List of Unexpected AEs
According to a blog post "
Seriousness, Expectedness and Investigator Brochures", there are actually two types of unexpectedness
The first is “regulatory expectedness”. This refers to the SAEs that the company considers likely/possibly or probably related to the study drug. This list is used to determine whether an SAE is a SUSAR (Suspected, unexpected serious adverse reaction) and thus expeditable to FDA, EMA and other health agencies.
The second we can call “clinical expectedness” which is a listing of SAEs that the investigator and patient may encounter during the trial and should be aware of. They may be due to the drug, the disease, comedications, concomitant illnesses (e.g. the flu) or other causes. These may or may not be the same as the “regulatory expectedness” list of SAEs but are important for the treating physician to be aware of and look for. It may not be possible yet to determine whether the particular SAE is due to the drug or the disease or comedications etc. This may become clearer later in the drug’s lifespan as more data becomes available; but sometimes it does not ever become clear.
Due to different understanding of the expectedness, different companies may act differently in handling the expectedness assessment. Some companies (especially the European companies) may want to add as many AEs as possible to the Investigator Brochure so that less AEs would meet the unexpected criteria – specifically the SUSAR criteria for expedite reporting.
Other companies may want to add as few AEs as possible to the Investigator Brochure because two many AEs listed in the Investigator Brochure would give the investigators an impression that the investigational product is not safe.
The right approach should be that the list of AEs/SAEs should be carefully reviewed by one or more medically qualified persons to decide if terms should be included (added) in the Investigator Brochure.
Expectedness assessment is more for fulfilling the sponsor’s reporting responsibility and expected / unexpected AEs are evaluated by the sponsor (not the investigators) through comparing to the Investigator Brochure or product label.
Expected AEs versus AEs of Special Interest (AESI)
Sometimes, the study protocol may include a list of AEs of Special Interest. According to FDA guidance for industry:
E2F Development Safety Update Report AEs of Special Interest are defined as following.
“Adverse event of special interest: An adverse event of special interest (serious or non-serious) is one of scientific and medical concern specific to the sponsor’s product or program, for which ongoing monitoring and rapid communication by the investigator to the sponsor can be appropriate. Such an event might warrant further investigation in order to characterize and understand it. Depending on the nature of the event, rapid communication by the trial sponsor to other parties (e.g., regulators) might also be warranted. (Based on CIOMS VI)”
Here are some examples of AESI: distal emboli events in clinical trials using thrombolytic agents, syncope events in pulmonary arterial hypertension studies, diarrhea in Irritable Bowel Syndrome studies) . I had a previous post "
Adverse Event of Special Interest (AESI), Standardized MedDRA Query (SMQs), Customer Queries (CQs), and SAS Programming"
AEs of Special Interest are usually the expected AEs.
An event can be an unexpected AE in the early development stage, but become the expected AE and AE of Special Interest in late stage. For example, during the TYSABRI® (natalizumab) (for multiple sclerosis) drug development, a rare brain infection—called progressive multifocal leukoencephalopathy (PML)— was unexpected in early stage, and then become an AE of Special Interest.