Randomization and blinding are two techniques to help prevent (conscious or unconscious) bias in clinical trials and they are the cornerstone of the randomized, controlled clinical trials (RCTs) and in FDA's terms, the cornerstone of the adequate & well-controlled clinical trials (A&WCs). As stated in FDA's
Randomization and blinding are the two principal means of reducing bias and ensuring
validity of trial conclusions. Randomization helps protect against the possibility that
differences between groups at baseline will lead to outcome differences that might
mistakenly be attributed to drug effect. Blinding protects against the possibility that
differences in the on-trial treatment or assessment of subjects will lead to spurious
outcome differences that are mistakenly attributed to a drug effect.
In the context of clinical trial design, randomization is defined as the allocation of
patients to the investigational drug and control arms by chance. Randomization is
intended to prevent any systematic difference between patients assigned to the treatments
being compared and is a critical assumption for valid statistical comparisons. It is also
intended to produce groups that are comparable (statistically balanced) with respect to
both known and unknown factors.
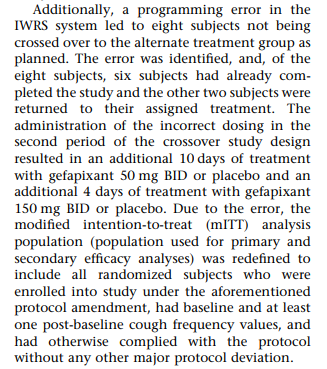
While every effort is made to prevent the mistakes in implementing the randomization, it is inevitable to have the randomization errors and mistakes here and there. Here are some of the randomization errors that may be seen in clinical trials.
Ineligible subjects are randomized: Clinical trials contain a screening period for verifying the eligibility of the study participants. All inclusion and exclusion criteria are checked during the screening period. If a subject meets all inclusion and exclusion criteria, the subject is eligible to be randomized. Sometimes, subjects are thought to be eligible for randomization, but only, later on, are found to be ineligible for one or more entry criteria. When ineligible subjects are randomized into the study and receive the assigned study treatments, the subjects are considered to be in the study. According to the intention-to-treat principle, the subjects will be included in the analyses regardless of the violation of the inclusion or exclusion criteria. If the critical criteria that are violated have an impact on the efficacy evaluation, the subjects may be excluded from the per-protocol population and sensitivity analyses are conducted with the per-protocol population to assess the robustness of the results from the primary analysis.
Choosing the wrong stratum for randomization: For clinical trials with stratified randomization, the randomization is executed within each stratum. When a new subject is eligible to be randomized, the next available randomization number in the corresponding stratum (for example, based on the subject's gender, baseline disease severity category,...) is allocated to the subject.
It is not uncommon that the investigational sites to select an incorrect stratum for the randomization especially when the strata information requires additional derivation and calculation, for example, if a subject with or without using one class of background medications is a stratification factor, the information about the use one class of background medication may need to be derived.
If a randomization stratification factor is measured more than one time, which measure will be used for randomization needs to be clearly stated in the protocol. If a spirometry parameter (for example, % predicted FEV1 >= 50% versus <50%) is used as a randomization stratification factor and spirometry tests are performed at both screening and baseline visits, the protocol needs to be specific regarding whether the results from screening visit or the baseline visit will be used for randomization - typically, the measures at the baseline visit should be used for randomization. If a laboratory parameter is used for randomization and there are both local lab and central lab, the protocol needs to be specific regarding which lab results will be used for randomization - typically the central lab results at the baseline will be used for randomization unless the central lab results can not be obtained in time for the randomization.
See previous post "Handling Randomization Errors in Clinical Trials with Stratified Randomization"
Randomize the patients too early before all eligibility criteria are met: The investigator rushed to go to the randomization system (IRT) and randomized the subject to trigger the downstream activities, then realized that one or more screening results were still pending.
Once the subject is randomized, it can’t be undone in the randomization system (IRT system). However, the site can hold on to the randomization information obtained and wait for the last pieces of the screening results to confirm the eligibility. If the last piece of the screening results confirms that the subject is eligible to be randomized, the previously obtained randomization information will then be used. The subject can move on to initiate the assigned study treatment. If the last piece of the screening results indicates that the subject is ineligible to be randomized, we will then need to decide if the subject is allowed to be in the study. If so, it will become the situation mentioned in the previous section "
Ineligible subjects are randomized".
In either situation, a protocol deviation needs to be recorded to document this
incident.
The PI was practicing the randomization system to see how the randomization works but accidentally randomized the subject in a live system. In this situation, there was no actual and real subject to be randomized. The subject information entered into the randomization system was not real, but one of the randomization numbers was assigned and treatment assignment was used.
While this subject may remain in the randomization system (IRT), the subject is fake and should be removed from the downstream clinical database. This is usually a rare event, therefore, has no big impact on the integrity of the original randomization.
Randomization system (IRT system) is down at the time of randomization or the internet is down: sometimes, the randomization needs to be performed immediately after the last eligibility criterion is confirmed. It is critical to have immediate access to the randomization information in order to randomize the subject in time for initiating the randomized treatment. However, it could happen that the IRT system is down or the internet is down when the randomization number and treatment assignments are needed.
If this is a situation, the advice is to have a backup manual randomization system (for example, calling an unblinded person or group).
Dispense the incorrect drug kit: nowadays, the randomization system is embedded in the system for clinical trial supplies (IRT system). In addition to the treatment assignments, a separate drug kit list will be generated. When a subject is randomized and a treatment group is assigned, the drug kits that are corresponding to the assigned treatment will be allocated and dispensed to the subject.
See a previous post "
Monitoring the double-blind study: unblinded pharmacist, unblinded monitor, and drug kit"
Due to human error, it is possible to have the correct randomization information but dispense the incorrect kit numbers. When this happens, it is adverse to verify with the clinical trial supply manager (who are unblinded) if the incorrect drug kit is for the same treatment group as the drug kit that is supposed to be dispensed (Don't communicate about the actual treatment group). It is less an issue if the incorrect kit numbers are in the assigned treatment group.
If the incorrectly dispensed drug kits are not in the assigned treatment group, the subjects received the incorrect treatment. For the statistical analysis, the subject will be included in the intention-to-treatment analysis and will be included in the randomized treatment group (so-called 'as randomized). The subject can be excluded from the per-protocol population for sensitivity analysis.
Recording the randomization date/time (local time versus backend system time): When a subject is randomized in the IRT system, a randomization message or printout, or randomization report will indicate the subject number, randomization number, the stratification factors used for randomization, randomization date/time. The investigator can record the randomization information in the case report form. Only blinded information can be included in the randomization report.
One issue for this report is the randomization date/time - is it based on the IRT system date/time or the local date/time? The local date/time should be used as the randomization date/time. If the IRT system is located in the UK and the subject is randomized in the US, the local and system time can differ in 5-8 hours. Local date/time, not the system date/time should always be used as the randomization date/time.
The same subject is randomized twice (unless it is the micro-randomized trial)
The majority of these randomization errors that occurred in the study were not included in the publications and regulatory submissions - the randomization issues appear to be less than what actually occurred. Some of the examples of the randomization errors can still be found in the literature:

"To start, at the beginning of CENTAUR, a randomization implementation problem
was identified and addressed by the unblinded statistician. Let’s walk through the
details.
In CENTAUR, kits were shipped one by one after successful screening visits.
While preparing for the first Data Safety Monitoring Board meeting in November
2017, the unblinded statistician found that the initial 18 study kits shipped were
all active. This was due to an error at the distribution center. They proceeded to
instruct the distribution center to balance these 18 kits by shipping a block of 9
placebo kits to maintain randomization.
After correction, the 2:1 active:placebo ratio was maintained.
The unblinded statistician notified Amylyx of this issue in January 2020, two
months after study unblinding in November 2019. Participants, investigators, and
study staff were never unblinded due to this error.
Upon notification, Amylyx initiated a thorough investigation of the root cause, in
consultation with the unblinded statistician and the distribution center. Amylyx
also consulted with external statisticians to determine the best approach to
assess the impact. The statisticians recommended a sensitivity analysis to exclude
the participants affected by the error."