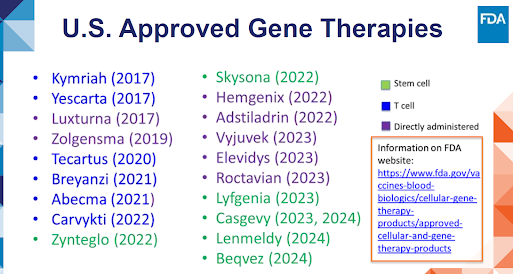
The FDA presentation by Dr Gopa Raychaudhuri, "Facilitating Development of Gene Therapies for Rare Diseases," summarized all Gene Therapies approved by the US FDA. There were 19 approved gene therapies: 6 stem cell therapies, 6 T cell therapies, and 7 directly administered therapies.
Gene therapy therapies are reviewed and approved by FDA Center for Biologicals Evaluation and Research (CBER), especially the Office of Therapeutic Products (OTP) - Approved Cellular and Gene Therapy Products are listed here.
|
Sponsor |
Product & Indication |
Study Design |
Sample Size |
FDA approval date/Brand Drug
Name |
|
Pfizer |
Adeno-associated
virus vector-based gene therapy. Adults with moderate
to severe hemophilia B. |
Phase 1/2a Study
C0371005 (Safety) - open-label,
single-dose, single-arm, multi-center. Phase 3 Study
C0371002 (Efficacy and Safety), open label, single-dose, multi-national study
. https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/beqvez |
15 subjects 45 subjects |
April 2024 Beqvez |
|
Orchard
Therapeutics |
Stem cell-based
gene therapy. Children with
pre-symptomatic late infantile, pre-symptomatic early juvenile, or early
symptomatic early juvenile, metachromatic leukodystrophy. |
Data from an
adequate and well-controlled investigation comprised of two single arm,
single-center, open-label studies, a European Union Expanded Access Program
(EAP), and one ongoing long-term follow-up study and a natural history study. https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/lenmeldy
|
Study
OTL-200-201222 (n=18) and Study 205756 (n=10) |
March 2024 Lenmeldy |
|
Vertex |
Stem
cell-based gene therapy-genome editing using CRISPR/Cas9 and SPY101. Patients aged 12 years and older with transfusion-dependent β-thalassemia (TDT). |
Multinational,
single-arm, open-label, phase 1/2/3 study. https://www.fda.gov/vaccines-blood-biologics/casgevy |
52 dosed, 35 evaluable. |
Jan 2024 Casgevy |
|
Vertex |
Stem cell-based
gene therapy -genome editing
using CRISPR/Cas9/SPY101 technology. Sickle cell disease in patients aged 12 years or older with recurrent vaso-occlusive crises. |
Multinational,
single-arm, phase 1/2/3 study. |
44 treated, 31 evaluable. |
Dec 2023 Casgevy |
|
Bluebird Bio |
LVV gene
therapy. Sickle cell disease in patients aged12 years or older with a history of vaso-occlusive events. |
Study Hgb
206, an ongoing Phase 1/2, open label, multicenter. https://www.fda.gov/vaccines-blood-biologics/lyfgenia |
Safety: 54
subjects. Efficacy: 32
subjects. |
Dec 2023 Lyfgenia |
|
BioMarin |
Adeno-associated
virus vector-based gene therapy. Adults with
severe hemophilia A. |
Open-label,
single-dose, single-arm, multinational phase 3 study. |
112 subjects
dosed and constituted the rollover population evaluated. |
June 2023 Roctavian |
|
Sarepta |
Adeno-associated
virus vector-based gene therapy. Ambulatory pediatric patients aged 4 through 5 years with Duchenne muscular dystrophy (DMD) with a confirmed mutation in the DMD gene. |
Open-label
study 101. Randomized, double-blind, placebo-controlled study 102. Open label study 103. |
Safety: 85
subjects. 73 subjects
received intended dose and 12 received lower doses. |
June 2023 Elevidys |
|
Krystal
Biotech |
Vector-based
gene therapy. Wounds in
patients 6 months of age and older with dystrophic epidermolysis bullosa with
mutation(s) in the collagen type VII alpha 1 chain (COL7A1) gene. |
First-in-human,
single-center, open-label, randomized, intra-subject, placebo (vehicle)
controlled phase 1/2 study (KB103-001). Multicenter, intra-subject randomized, placebo-controlled, double-blind open-label phase 3 study (B-VEC-03). https://www.fda.gov/vaccines-blood-biologics/vyjuvek |
9 subjects. Safety: 31
subjects. |
May 2023 Vyjuvek |
|
Ferring
Pharmaceuticals A/S |
Vector-based
gene therapy. Adult patients with high-risk Bacillus Calmette-Guérin unresponsive non-muscle invasive bladder cancer with carcinoma in situ with or without papillary tumors. |
Single-arm
trial study (CS-003). https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/adstiladrin |
107 subjects
enrolled. 98 subjects
evaluable. Efficacy: 55
subjects. |
Dec 2022 Adstiladrin |
|
CSL Behring |
Adeno-associated
virus vector-based gene therapy. Adults with
Hemophilia B (congenital Factor IX deficiency). |
Open-label,
single-dose, single-arm, multi-center phase 2b study. Open-label, single-dose, multi-center, multinational phase 3 study. https://www.fda.gov/vaccines-blood-biologics/vaccines/hemgenix |
3 subjects. 54 subjects. |
Nov 2022 Hemgenix |
|
Bluebird bio |
Stem cell-based
gene therapy. Slowing the progression of neurologic dysfunction in boys 4-17 years of age with early, active cerebral adrenoleukodystrophy. |
Open-label,
multicenter, single-arm phase 2/3 study. Open-label, multicenter, single-arm phase 3 study. https://www.fda.gov/vaccines-blood-biologics/skysona |
Safety: 67
subjects. Efficacy: 61
subjects. |
Sept 2022 Skysona |
|
Bluebird Bio |
LVV Gene
Therapy Beta-thalassemia. B cell
maturation antigen-directed genetically modified. Adult and pediatric patients with ß-thalassemia who require regular red blood cell (RBC) transfusions. |
Two
open-label, multicenter, single-arm phase 3 studies. https://www.fda.gov/vaccines-blood-biologics/zynteglo |
18 in HGB-212
study and 23 in HGB 207 study. |
Aug 2022 Zynteglo |
|
Janssen
Biotech |
Autologous T
cell immunotherapy. Adult patients with relapsed or refractory multiple myeloma who have received at least one prior line of therapy. |
Single-arm,
phase 1b-2 multicenter study. https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products/carvykti |
Efficacy: 97
subjects. |
Feb 2022 Carvykti |
|
Celgene
Corporation |
B cell
maturation antigen-directed genetically modified autologous T cell
immunotherapy. Adult patients with relapsed or refractory multiple myeloma after two or more prior lines of therapy including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody |
Single-arm,
multicenter phase 2 study. https://www.fda.gov/vaccines-blood-biologics/abecma-idecabtagene-vicleucel |
Safety: 127
subjects. Efficacy: 100
subjects. |
March 2021 Abecma |
|
Juno
Therapeutics |
CD19-directed
genetically modified autologous T cell immunotherapy. Adult patients with large B-cell lymphoma, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B. |
Single-arm,
multicenter phase 1 study. |
Safety: 268
subjects. Efficacy: 256
subjects. |
Feb 2021 Breyanzi |
|
Kite Pharma |
CD19-directed
genetically modified autologous T cell Immunotherapy. Adult
patients with relapsed or refractory Mantle Cell
Lymphoma. |
Single-arm,
multicenter, phase 2 study. |
68 subjects
treated. Efficacy: 60
subjects. |
July 2020 Tecartus |
|
AveXis |
Adeno-associated virus vector-based gene therapy. Pediatric
patients less than 2 years of age with spinal muscular atrophy (SMA) with
bi-allelic mutations in the survival motor neuron 1 gene. |
Open-label,
single-arm, ascending-dose, phase 1 study. Open-label, single-arm, phase 3 study. |
15 subjects. 44 subjects. |
May 2019 Zolgensma |
|
Spark
Therapeutics |
Adeno-associated
virus serotype 2 vector gene therapy. |
Open-label, dose-escalation,
phase 1 study. Open-label, randomized, controlled, cross-over, phase 3 study. |
12 subjects. 29 subjects. |
Dec 2017 Luxturna |
|
Kite Pharma |
CD19-directed
genetically modified autologous T cell
immunotherapy. Adult patients with large B-cell lymphoma that is refractory to first-line chemoimmunotherapy or that relapses within 12 months of first-line chemoimmunotherapy |
Single-arm,
open-label, multicenter phase 1/2 study. |
Safety: 108
subjects. Efficacy: 101
subjects. |
Oct 2017 Yescarta |
|
Novartis
Pharmaceuticals |
CD19-directed
genetically modified autologous T cell immunotherapy. Adult patients with relapsed or refractory follicular lymphoma after two or more lines of therapy. |
Multicenter,
open-label, single-arm, trial. |
63 subjects. |
Aug 2017 Kymriah |