CQ's web blog on the issues in biostatistics and clinical trials.
Sunday, July 28, 2024
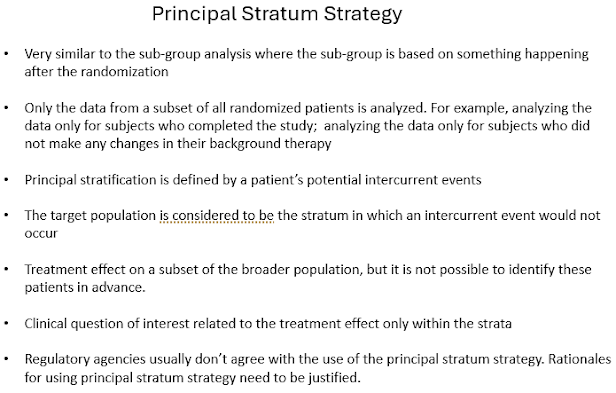
Five most frequently used strategies for handling intercurrent events
Wednesday, July 24, 2024
Clinical trial succussed in phase 2, but failed in phase 3
The Reality Check of Phase 3
Phase 3 trials are more extensive, involving several hundred to several thousand participants. These trials are designed to confirm the efficacy and safety of the treatment on a larger scale, comparing it directly to existing standard treatments or placebos. Phase 3 trials are pivotal because they provide the comprehensive data needed for regulatory approval- so called 'licensure trial'.
Despite the promise shown in Phase 2 study, many treatments fail in Phase 3 study. The reasons for these failures are multifaceted and can be broadly categorized into four main areas:
Differences in Population and Scale:
- Population Diversity: Phase 2 trials often involve more homogeneous patient groups, while Phase 3 trials encompass a broader and more diverse population. This diversity can introduce variables that were not accounted for in the smaller, more controlled Phase 2 trials. For example, genetic differences, comorbidities, and concurrent medications can all influence treatment outcomes.
- Sample Size: The larger sample size in Phase 3 trials can reveal less common side effects or variations in treatment efficacy that were not apparent in Phase 2. What appeared as a clear benefit in a smaller group may not hold up when tested on a larger scale. The large sample size requires more clinical trial sites for patient enrollment and the study needs to be designed as the multi-regional clinical trial.
Study Design and Execution:
- Study Rigidity: Phase 3 trials often have more rigid protocols and endpoints compared to Phase 2. The stringent criteria and predefined outcomes might not fully capture the treatment’s potential benefits, leading to negative results. Phase 3 trials are usually more statistically rigor. More stringent statistical analysis approaches are used in the analyses of the phase 3 study data including controlling type-1 error, adjustment for multiplicity, missing data handling, estimands and strategies for handling the intercurrent events...
- Execution Challenges: The complexity of conducting large-scale trials can introduce logistical issues, variations in study conduct across different sites, and difficulties in maintaining consistent treatment administration. Execution challenges may also include the difficulties in patient retention, treatment compliance, and maintaining the treatment blinding,...
Efficacy and Endpoint Discrepancies:
- Efficacy Overestimation: Positive results in Phase 2 might be due to smaller sample sizes, shorter follow-up periods, or more lenient statistical thresholds. When scaled up, the actual efficacy might be less impressive.
- Endpoints and Metrics: The primary and secondary endpoints in Phase 3 trials may differ from those in Phase 2. A treatment might show improvement in a specific metric in Phase 2 but fail to meet the broader, more comprehensive endpoints required in Phase 3. Phase 2 study may be based on surrogate endpoints and biomarkers while phase 3 study needs to use the endpoints that measure patients' feel, function, and survival to meet the regulatory requirements. Phase 2 study is usually shorter in duration while phase 3 study is usually longer.
Unanticipated Safety Concerns:
- Rare Adverse Events: Larger trials can uncover rare but serious adverse events that were not evident in the smaller Phase 2 trials. These safety concerns can overshadow the benefits observed, leading to a failed trial.
- Long-Term Effects: Phase 3 trials typically have longer follow-up periods, which can reveal long-term side effects or diminishing efficacy over time.
"There are many reasons that potentially efficacious drugs can still fail to demonstrate efficacy, including a flawed study design, an inappropriate statistical endpoint, or simply having an underpowered clinical trial (i.e., sample size too small to reject the null hypothesis), which may result from patient dropouts and insufficient enrollment."
Here are two new examples with promising phase 2 study results, but failed phase 3 study:
"...Prompted by these negative results, a post hoc reevaluation of the phase II trial revealed that the apparent benefit of zinpentraxin alfa was primarily driven by two outliers in the placebo group who had an FVC decrease of more than 2,000ml/yr."